It's time to prepare for your first prenatal visit when you're plus size and pregnant.
Things look slightly different when you have a BMI over 30. So, we're here to go beyond basic information around what to expect during your first prenatal visit, so you'll truly feel prepared.
Please note, that none of the information in this article should be interpreted as medical advice. Always talk to your care provider about any questions or concerns you may have!
Disclosure: Plus Size Birth is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program. As an Amazon Associate, I earn from qualifying purchases. Read more about these links in my disclosure policy.
Before You Go To Your Plus Size Prenatal Visit
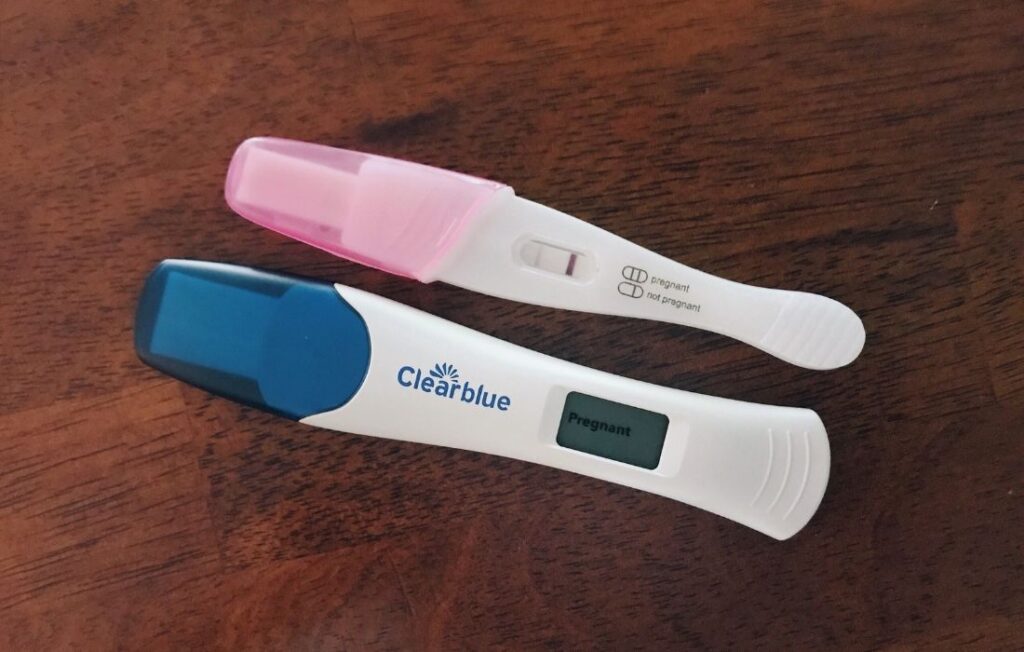
It's common to think you'll go in for your first prenatal visit right after getting a positive pregnancy test. So it might be surprising to learn most people don't have their first visit until six to eight weeks of pregnancy – and sometimes even closer to twelve weeks!
With that said, if you're under the care of a fertility specialist or have any health concerns, you might be seen sooner than six weeks.
3 Important Questions To Ask
When you're ready to book your first prenatal appointment, consider asking the following questions.
Do you have any BMI restrictions?
Many birth centers and some midwifery and doctor practices have BMI restrictions.
It can be frustrating and upsetting to go in for an appointment only to learn you can not receive care because of your size. So, asking ahead of time can make sure you don't get caught off-guard when you arrive.
Most physician practices do not have BMI cut-offs. However, many set guidelines for patients with a BMI over 40 (and sometimes for those with a BMI over 30).
For example, you might be told you need to have a consult with a maternal-fetal medicine specialist. Some providers will also encourage their plus size patients to consent to an induction at 39 weeks.
So, even if your selected care provider doesn't have any BMI restrictions, inquire if they will recommend additional testing, appointments, or procedures due to your BMI.
Please note that it's perfectly okay if you want additional screening throughout your pregnancy, but you might need to switch care providers if you don't.
Do you have large gowns and blood pressure cuffs?
These are two things that should be standard in all care provider offices but are not always.
You can bring your own gown if that makes you feel more comfortable – but you shouldn't have to!
Care providers should have the blood pressure cuff sizes needed to support patients of all sizes. If they don't, it's a major red flag that they are not size-inclusive.
At which hospital would I be giving birth if I see your providers?
Unless you're having a home birth, you'll want to research your selected care provider and where you plan to give birth.
Some medical facilities and birth centers have BMI restrictions for water birth and access to the midwifery model of care. There are also facilities that have monitors for laboring that work much better on larger bodies. As well as, hospitals that are better equipped to take care of plus size pregnant people.
So, be sure to research your selected facility, along with your care provider!
Download your copy of the My Size-Friendly Care Provider's Guide. It goes into things to look out for and additional questions to ask!
Talk To Your Partner Or Support Person
Many studies show a care provider bias against people of size. So, you might already have experienced what it feels like to be mistreated by a care provider.
Because of this, I encourage you to talk with your partner or a supportive friend or loved one about your desire to make sure your care provider is fat-friendly. And hopefully, they can join you for prenatal visits.
That way, your go-to person can be an extra set of eyes and ears during your visit. They can look out for many of the things mentioned here and throughout the Plus Size Birth website.
Don't worry if you're planning to go to doctor visits alone either; we still have you covered!
When You Arrive
You're going to be spending a lot of time at this doctor's office, especially near the end of your pregnancy. So you want to feel as comfortable as possible!
Pay close attention to how the staff treats you and if the office is size-inclusive – from chairs without arms so you can sit comfortably, to the use of that larger blood pressure cuff (if needed).
During Your Prenatal Visit
We'll break your prenatal visit into three parts: medical and family health history, physical exam, and patient education.
Medical And Family Health History
A nurse or medical assistant will ask you a lot of questions to take a complete medical and family health history.
You'll want to be as honest as possible in answering these questions.
Now is also the optimal time to share if you've experienced weight stigma by care providers in the past, or if you’re concerned about the possibility. You can even ask to have it noted in your file so that other members of the medical team know to be sensitive to this previous experience.
Physical Exam
A quick note on hygiene before we move on.
Just like the information you'll read in nearly every article on well-women visits, there's no need to shave, wax, or even trim your pubic hair.
So with that out of the way, let's talk about another worry people have but don't often talk about – sweat and odor. Everybody sweats and every body has a smell!
If you're concerned about being sweaty, you can throw a pack of baby wipes or bathing wipes in your bag. Then do a quick wipe-down before your exam while you're changing into a gown. This sure isn't something you have to do to make anyone else feel comfortable. It's just a suggestion in case you are someone who would feel more confident after using a wipe.
You can also request an absorbent pad to sit on (known as a chux pad), rather than the usual paper on the exam table.
Moving on, when taking your vitals at this and every prenatal appointment (and at regular doctor's visits moving forward), here are some helpful tips for plus size people.
Giving A Urine Sample
You'll likely need to provide a urine sample to confirm your pregnancy before your prenatal visit starts.
Heads up if you haven’t done it before – this often messy task is one you'll need to master. You'll provide a urine sample at every prenatal visit moving forward.
When you're plus size, it can be harder to reach to hold the tiny cup, especially if you have an apron belly.
If you’d like to have an alternative, a urine catch basin makes providing a sample far easier! You can ask your provider if they carry them or even order your own in bulk from Amazon to bring with you to appointments.
Just note that re-using a urine catch basin can affect test results.
Getting Weighed
Stepping on the scale is something many people dread. So, you're not alone if this is your least favorite part of going to your doctor.
More and more people are refusing to be weighed. As a mentally competent adult, you don't have to consent to any medical measurement, test, or procedure that you don't want to do. Nothing is mandatory!
With that said, having your weight recorded is just one of many measurements to see how your body is navigating your pregnancy. And especially during this first prenatal visit, it might be useful to get a baseline.
If there's a sudden increase or decrease in weight, this alerts your providers of different potential medical complications. And if you plan to have an epidural in labor or require other medications, your care providers will need to know your weight in order to determine appropriate dosages for the health and safety of you and your baby.
We encourage you to have an open mind about standing on the scale and know you have options.
Options For Getting Weighed
- You can ask for the number not to be said aloud. Thankfully this doesn't happen often, but it can alleviate some anxiety when making this request.
- Feel free to look away rather than at the number on the scale. Or you can stand backward on the scale! It might feel silly at first, but you'll get used to it quickly. Plus, know this is something many people do, but it doesn't get talked about often.
- Ask to be weighed privately if the scale is in a very public area of the office.
- If you don't want to stand on the scale when you first get called back, you can say you'd like to wait until you're ready.
- Weigh yourself at home, and be prepared to say that number aloud or have it written down to share.
You might get some pushback with this last option or if you decide not to stand on the scale at all. Therefore, it's critical to have an open and honest conversation with your care provider regarding being weighed and any concerns you have.
Having Your Blood Pressure Taken
Getting an accurate blood pressure reading requires using the correct size cuff for your body.
Often plus size people need a larger cuff. However, many medical offices don't have different size cuffs in each exam room. So, be sure to speak up!
Also, if you're feeling nervous at your doctor's visit, you can ask to have your blood pressure taken at the end when you feel calmer. Far too often, people are rushed back to the exam room after being weighed. And, before they catch their breath, the cuff is wrapped around their arm.
There are guidelines for having your blood pressure measured, including being seated for at least five minutes with your feet firmly planted on the floor. Sitting with crossed legs (or even ankles) or talking, can make your blood pressure read higher.
Learn more about advocating for the correct size cuff, and don't be embarrassed to speak up if necessary. Just don't forget to remind the medical assistant if you’ve asked to delay getting this vital taken. Waiting till the end will be out of their ordinary routine and you don’t want to skip it by accident!
Note for the future: if you have non-stress tests, be sure your blood pressure is taken when seated and not lying down for a more accurate reading. This might require you to advocate for a chair to be brought in and for the medical staff to wait until you have been seated for five minutes.
It is unfortunately often the case that rooms are poorly set up to follow these guidelines but an accurate reading of your blood pressure is important and you should always feel comfortable asking for the care you deserve!
Blood Tests
Blood tests can tell us a lot about your overall health. Also, these tests allow for genetic screening and gathering information about the sex of your baby.
During this visit, your care provider may order multiple blood tests. So, be prepared for that and make sure you're well-hydrated. Speaking of tests, be sure to learn about noninvasive prenatal screening, and how it can be different when you have a high BMI.
If those chairs designed for giving blood are a tight squeeze, you can advocate for the phlebotomist (the person taking your blood) to raise the armrest. Your belly should have more room, and the armrest should lay flat by doing this.
If you're still uncomfortable, ask for additional accommodations, such as drawing your blood in the exam room.
If someone has trouble finding and accessing your veins with multiple attempts, speak up and ask for another phlebotomist. The same goes if anyone makes inappropriate comments about your body – you deserve to be treated with dignity!
Pelvic Exam
You're probably used to seeing ultrasounds happening on the outside of the belly. For your first prenatal visit (and possibly a few others), the recommendation will be to have what is called a transvaginal (TV) ultrasound. And this is for people of all sizes, not just when you’re plus size.
To have a TV ultrasound, you will lay down on an exam table, bring your bottom down to the end of the table (it will feel almost like you will fall off!), and have your feet in stirrups.
The ultrasound device is a long wand, and it's inserted vaginally to provide a view of your uterus (and what's inside).
Some people find these types of ultrasounds to be invasive and uncomfortable. So, make sure you talk to whoever is performing the ultrasound to have a clear sense of what to expect. In addition, have a plan to have them stop if you need a break. And as always, nothing is mandatory.
Listen to the interview below with an ultrasound technologist during episode 165 of the Plus Mommy Podcast to learn more about preparing for ultrasounds when you're plus size.
Along with the transvaginal ultrasound, you can expect a recommendation for a pelvic exam. As well as possibly a pap smear if you haven't had one in a while. This exam also occurs while you lay on your back with your feet in stirrups.
Often a provider will use their fingers and a speculum (a tool to open your vagina to see your cervix). Again, talk to your provider about any concerns. You can ask to have a support person with you if that helps, and make a plan to have the exam stop if you need that at any point.
During your transvaginal ultrasound, you might hear your baby's heartbeat for the first time. That's something to look forward to hearing!
Patient Education
During this portion of your first prenatal visit, your care provider has a lot of things they will likely want to share with you about your physical and mental health and maintaining a healthy pregnancy.
There are specific evidence-based recommendations the American College of Gynecologists and Obstetricians (ACOG) has for people with a BMI over 30. Your provider's office will have its own guidelines and safeguards as well.
During your prenatal visit, your care provider should have a conversation about any recommendations based on your BMI in an unbiased manner. This allows you to make the choices that best suit your situation.
Below you'll see some standard recommendations, but be sure to ask your provider how they care for patients with a high BMI; that way, you'll know what to expect.
Also, consider having someone come to your appointment with you as this sometimes makes it easier to remember to ask questions or take in all the information shared with you. This could be a partner, a family member, a friend, or a doula if you have one.
Counseling for Increased Risks During Pregnancy
Studies show that people with a BMI over 30 can have increased risks during pregnancy, including incurring gestational diabetes, preeclampsia, fetal macrosomia (big baby), preterm labor, miscarriage, and stillbirth.
It's never easy to read that list. But, the fact remains that most plus size people who go into pregnancy healthy also have healthy pregnancies. You’re more likely to have a healthy pregnancy than a complicated one, statistically speaking. And, nothing on that list happens only to plus size people. So often we're talking about a relatively small increase in risk.
It's essential to understand the difference between relative risk (comparing one risk to another) and your actual risk factor.
Speaking of risks, now's a critical time to ask your care provider if they will classify you as high-risk based on your weight alone. There are many reasons why people are classified as high-risk during pregnancy, but ACOG does not recommend that label for people based solely on BMI.
What does this mean for you? If all other indexes of your health are normal, being labeled as high risk is likely both unnecessary and might lead to restrictions that are not appropriate for you.
For example, being labeled high risk might mean extra testing and a recommendation for earlier labor induction. As well as restrictions on things like laboring in the shower or having more mobility during labor.
If you desire every test possible and want extra ultrasounds – that's great!
If you don't want additional screening unless it’s medically indicated – that's fine, too!
You want to make sure you're on the same page with your care provider. So, be sure to have this conversation early on in the pregnancy so you are not surprised.
Regardless of your classification, you'll also want to know if your care provider will ask you to do additional testing and refer you to other specialists (from maternal-fetal specialists to cardiologists, if need be). It's never appropriate for things to be sprung on you by your provider.
Communication is key for the provider-patient relationship!
Early Pregnancy Screening for Glucose Tolerance
In 2013, the ACOG recommended early screening for diabetes for those with a BMI over 30. For many care providers, this has become a standard of care.
This early glucose screening doesn’t actually check for gestational diabetes.
The early glucose tolerance test recommendation was made because people with a BMI over 30 have a greater risk of being pre-diabetic or diabetic. And they might not yet have been diagnosed.
However, in 2020 it was discovered that early screening has not made a significant difference. So, if you were recently tested for diabetes, or don’t have a family history of diabetes, you can talk with your provider. See if this early screening is necessary, especially in light of recent data.
Weight Gain Recommendations
While there can be potential increased risks during a plus size pregnancy, as we shared above, studies also show that one way to reduce risks is to limit weight gain during pregnancy.
When you have a BMI of 30 or higher and are carrying one baby, the recommended weight gain is 11 – 20 pounds. For twins or multiples, the number increases to 25 – 42 pounds. There isn’t a lot of data to support these specific numbers but this is the current recommendation.
We know that can feel overwhelming!
Any talk of weight or mention of pounds can feel emotional for some people. Just know it's common for plus size people who are proactive with nutrition and physical activity not to gain much weight during pregnancy. Some people even lose weight, but that shouldn't be a focus (and dieting during pregnancy should never be encouraged).
Your care provider will talk about being physically active throughout pregnancy. They will also go over basic nutritional information and may refer you to a nutritionist. Try to connect with a Health At Every Size® informed nutritionist or dietitian.
If you are nourishing yourself with nutrient-dense food and you are able to get regular movement, this is key to a healthy pregnancy, regardless of the numbers on the scale.
We hope this conversation about weight happens in a way that is supportive and affirming, not stigmatizing or shaming. Remember, it’s okay to advocate for yourself! Whenever possible, voice your discomfort to your provider if they’re using language that feels unkind or unhelpful.
Final Thoughts
We highly recommend you arrive prepared for your first prenatal visit with questions. This is why we have a recommended list for Q&A in our My Size-Friendly Care Providers Guide.
You might love the provider you see during your first visit. But it's important to note care providers often rotate through on-call schedules for attending births. If this is the case for you, be sure to try to meet with each provider before your estimated due date (if the practice will allow you to do this).
Also, while it's not always easy, you can switch your care provider at any point. If you’re feeling unsupported and you’re not being heard, know that you and your baby are worthy of exceptional medical care. Whenever possible, seek out other local options for care if the first provider is not the right match.
We hope this information helps your first prenatal visit go smoothly, and you connect with an incredible size-friendly care provider!
References
- Nagpal, T. S., da Silva, D. F., Liu, R. H., Myre, M., Gaudet, L., Cook, J., & Adamo, K. B. (2021). Women's Suggestions for How To Reduce Weight Stigma in Prenatal Clinical Settings. Nursing for Women's Health, 25(2), 112-121. doi:10.1016/j.nwh.2021.01.008
- Dejoy, S. B., & Bittner, K. (2015). Obesity stigma as a determinant of poor birth outcomes in women with high BMI: A conceptual framework. Maternal and Child Health Journal, 19(4), 693-699. doi:10.1007/S10995-014-1577-X
- Gudzune, K. A., Beach, M. C., Roter, D. L., & Cooper, L. A. (2013). Physicians build less rapport with obese patients. Obesity, 21(10), 2146-2152. doi:10.1002/oby.20384
- Poon, M., Tarrant, M (2009) Obesity: attitudes of undergraduate student nurses and registered nurses doi: 10.1111/j.1365-2702.2008.02709
- Ceglowski, P., Lehane, K., Chow, C., Pelecanos, A., Tognolini, A., & Eley, V. (2020). Arm Dimensions of Patients with Obesity and Their Experiences with Blood Pressure Measurement: An Observational Study. Obesity (Silver Spring), 28(4), 718-723. doi:10.1002/oby.22746
- Dashe, J.S., McIntire, D.D. and Twickler, D.M. (2009), Maternal Obesity Limits the Ultrasound Evaluation of Fetal Anatomy. Journal of Ultrasound in Medicine, 28: 1025-1030.
- ACOG Committee opinion no. 549: Obesity in pregnancy
- Champion, M. L., & Harper, L. M. (2020). Gestational Weight Gain: Update on Outcomes and Interventions. Current diabetes reports, 20(3), 11.
- S. Joy, N. Istwan, D. Rhea, C. Desch, and G. Stanziano, (2009) The Impact of Maternal Obesity on the Incidence of Adverse Pregnancy Outcomes in High-Risk Term Pregnancies, American Journal of Perinatology, vol. 26, no. 5, pp. 345–349, 2009.
- Harper LM, Jauk V, Longo S, Biggio JR, Szychowski JM, Tita AT. (2020) Early gestational diabetes screening in obese women: a randomized controlled trial. Am J Obstet Gynecol. 2020 May;222(5):495.e1-495.e8. doi: 10.1016/j.ajog.2019.12.021
- ACOG Committee opinion no. 548: Weight Gain During Pregnancy
- Rasmussen, K. M., Yaktine, A. L., & Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines (Eds.). (2009). Weight Gain During Pregnancy: Reexamining the Guidelines. National Academies Press (US)
- Cooper DB, Yang L. Pregnancy And Exercise. (2021) In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2021. PMID: 28613571.
- Muktabhant B, Lawrie TA, Lumbiganon P, Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 6. Art. No.: CD007145.
- Gestational Diabetes Diagnosis: What Now? A Helpful To-Do List! - October 18, 2023
- Navigating Miscarriage and Self-Blame as a Plus-Size Individual - October 16, 2023
- How much does your BMI increase the odds of shoulder dystocia? - August 11, 2023