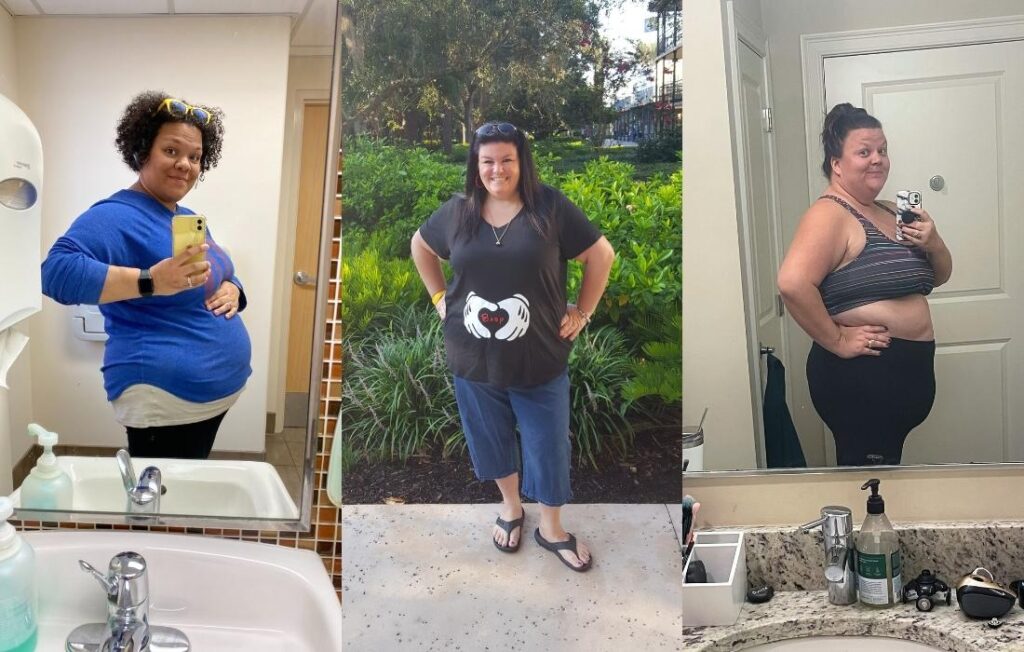
Are you trying to conceive and want to research first trimester plus size pregnancy week by week? Or did you just find out you're pregnant? Welcome, you're in the right place!
Below, we share helpful information you can use throughout the first 13 weeks of a plus size pregnancy.
Disclosure: Plus Size Birth is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program. As an Amazon Associate, I earn from qualifying purchases. Read more about these links in my disclosure policy.
First Trimester Quick Overview
None of the information on this website or our social media outlets should be interpreted as medical advice. Always talk to your care provider about any questions or concerns you may have!
This plus size first-trimester pregnancy resource isn't a substitute for your favorite pregnancy app or weekly email from sites like Baby Center.
We don't cover a lot of the essential topics you'll find there. For example, you won’t hear from us that your baby is the size of a papaya on any given week. However, we cover sweet tips to help you feel informed when you have a pregnancy in a plus sized body. As well as where to find plus size maternity clothes!
This plus size first-trimester pregnancy resource is for those with a BMI of 30 and above. We'll walk you through everything you need to know with evidence-based information shared in a positive rather than stigmatizing manner.
While Body Mass Index (BMI) is a flawed and inaccurate calculation of health, it's the current standard used in healthcare. BMI classifies people as underweight, normal weight, overweight, or obese.
Knowing your BMI and how it impacts pregnancy is essential. To calculate BMI you take a person's height divided by their weight.
It’s important to note, just because there are some increased risks – it doesn't mean you'll experience everything we'll address.
Plus size people overwhelmingly have healthy and uncomplicated pregnancies, especially when they are able to access size-friendly providers.
Plus Size First Trimester Pregnancy Breakdown
None of the information on this website or our social media outlets should be interpreted as medical advice. Always talk to your care provider about any questions or concerns you may have!
Week 1: Determining Your Due Date
Technically, you're not pregnant yet, but healthcare providers use your last menstrual cycle to determine your estimated due date.
So, let's take this opportunity to talk about a few things related to being plus size and trying to conceive. Along with how these things might play into determining your due date once your pregnancy is confirmed.
Unless you've been actively tracking your menstrual cycle or getting fertility support, you likely don't know exactly when you ovulated. Also, some plus size people have irregular cycles due to hormonal imbalances. This can especially be the case if you have Polycystic Ovarian Syndrome (PCOS).
Because of this, when you learn you're pregnant, you might wind up being further along than you thought. Don't worry, your care provider will confirm your estimated due date via ultrasound.
And please remember, people of any size can have irregular cycles and PCOS!
If you're currently trying to conceive, be sure to schedule a preconception appointment with a size-friendly care provider. You'll also want to start taking a prenatal vitamin with folic acid, and focus on your overall wellness.
We're crossing our fingers for your BIG FAT POSITIVE pregnancy results to show up soon!
Week 2: Pregnancy Symptoms
It's week two of pregnancy, and if you've conceived, it's that time when the egg meets the sperm. And then everything you learned way back in sixth-grade health class starts to occur.
Now is a prime time for us to talk about plus size pregnancy symptoms. It’s around this time that your hormones are shifting, and you might begin feeling “different” within a week or so. But if you feel completely normal, don’t fret; most pregnancy symptoms don’t hit hard until around week six when your hCG levels peak (more on that soon).
When it comes to plus size early pregnancy symptoms, they are the same for people of all sizes. You might experience a stronger sense of smell, unfamiliar cervical mucus, breast soreness, exhaustion, and a pelvic ache… along with a general moodiness or irritability.
The confusing thing is all of these symptoms can also occur when you're about to start your menstrual cycle. And these symptoms can be easily missed if you're not in tune with your body or just have a busy week at work.
Hang-tight. Lots of exciting things are happening, even if you’re unaware!
Week 3: hCG Levels
While it's still super early, around the end of this week is when people often take a pregnancy test.
So, it's time we address something that might be disappointing to hear. Pregnancy tests don't work as well very early on for larger-bodied people.
Why is that the case? Good question!
When you dip the pregnancy test into your urine, it detects the presence of a hormone called human chorionic gonadotropin (hCG).
Studies show that plus size people have lower hCG levels. This doesn't mean there's anything wrong with your body. These tests were not created with plus size bodies in mind so they do not always work.
In the same way plus size people need a little extra time during the first stage of labor (don’t worry, more info coming on that during the third-trimester), you also might want to wait a few additional days before taking a pregnancy test.
Now, we know days feel like weeks when you're not sure if you're pregnant or not. So, by all means, if you want to test – then test!
You might get that positive result right away. But if you don't, you might still be pregnant. Just remember to breathe – it’s good practice for parenthood anyway.
Thankfully, hCG levels typically double every two to three days – such an amazing rate. As your hCG rates increase, so will the effectiveness of home pregnancy tests.
You'll likely know if you're pregnant after waiting to test just a few short days following the first day of your missed period.
Quick tip! Did you know that Dollar store tests are just as accurate as any other test? And if you're testing out of “I just need to test,” then you can run through a bunch of them. So, don't pay $15 a test if you don't need to! You can even purchase testing strips in bulk via Amazon.
Week 4: Size-Friendly Healthcare Providers, Nutrition, & Physical Activity
You’re pregnant! You should have that positive pregnancy test by the end of this week, if not sooner.
We know that the next six weeks are critical for your baby's development. Unlike ever before, now's the time to tune in to your body.
If you Google “obesity in pregnancy,” you'll face a lot of information that might feel highly discouraging and even scary. For example, you'll read you're at a much greater risk for gestational diabetes. And that you shouldn't gain a lot of weight. This information can come from biased sources and paints an overly negative picture.
In the words of Taylor Swift, shake it off!
We're going to cover all of those topics above so you get the information you need. But we’ll present this information in a way that encourages you to feel proactive with your wellness rather than defeated or ashamed.
Our three keys for having a healthy plus size pregnancy are to connect with a size-friendly healthcare provider, eat foods that nourish your body, and find a movement practice that feels good (and that you look forward to doing).
Connect with a Size-Friendly Healthcare Provider
One of the most significant differences we've found in how a plus size person feels about their pregnancy is the type of care they receive.
Whenever possible, you want to connect with a size-friendly care provider. It’s so important to try to find a provider who believes you can have a healthy pregnancy. And someone who wants to support you with care that is individualized. And we have a guide you can download right now on how to do just that!
Nourish Your Body
For people of all sizes, pregnancy is a time to pay attention to nutrition and physical activity. Being proactive with both can reduce the chances of developing pregnancy complications.
Many people have a history of disordered eating. And your care provider will likely address weight-gain limits during your pregnancy that can be triggering (more on that soon).
Please know you're not alone if you've struggled with this.
Pregnancy is NOT a time to diet; it's an opportunity to transform your relationship with food.
The American College of Gynecologists and Obstetricians (ACOG) recommends people with a BMI over 30 get a referral to a nutritionist. So, don't be surprised if this comes up at your first prenatal visit. This referral can be useful for help with nutritional information and meal planning ideas. You can even say you don't want to talk about weight.
We recommend connecting with a Health At Every Size® (HAES®) aligned nutritionist whenever possible. It can be a truly positive experience to work with a nutrition expert who has addressed their size bias. And someone who is aware of the harmful impacts of diet culture. You might really enjoy talking with a provider who supports your health in the body you have!
To find a HAES®-aligned nutritionist, simply Google “HAES nutritionist” and your city. Other search terms are Health At Every Size dietitian, anti-diet nutritionist, and intuitive eating counselor. Many folks also work remotely! So, you might find a telehealth option in another city if no one is available locally.
Along with your overall nutrition, you'll also want to be aware of any vitamin deficiencies. Plus size people have a higher risk of being deficient in Iron, Folic acid, vitamin D, and B12.
Be sure to talk to your care provider about testing your vitamin and iron levels. You'll also want to discuss taking additional vitamins and supplements.
For those who are pregnant after a weight loss surgery, you'll want to work closely with your care team. They'll need to monitor nutrition and vitamin deficiencies throughout pregnancy and postpartum. These surgeries can increase the need for supplements.
Move Your Body in Joyful Ways
Physical activity helps your body stay healthy, boosts your mood, and builds stamina for labor and parenthood. So it's a win-win!
For physical activity, we ask: what brings you joy?
You might already have an exercise or movement routine you love. But if you don't, we have a lot of helpful suggestions for exercising during a plus size pregnancy. We even have ideas for things you can do at home.
Generally, your care provider will say you can continue with whatever activity you were doing before becoming pregnant. However, if you're looking to add new activities, that's great, but consider running new ideas past your provider.
Beyond all the awesome endorphins that are released when you're physically active, you'll also get a better night's rest. And that's priceless!
You've Got This
For your 5th week of pregnancy, we'll prepare you for your first prenatal visit. But, for now, we hope you'll dig into our guide on how to connect with a size-friendly care provider. Then, tap into helpful information about nutrition that's not tied to dieting. Finally, start a movement routine if you don't have one already. Going for a short walk while jamming to music from the 90s is a great starting place!
Be sure to take things at your own pace. We understand this is possibly a significant shift in your life. So, you don't need to do everything all at once.
So, be kind to yourself along this journey, and get lots of rest – you’re growing a tiny human, after all!
Week 5: First Prenatal Visit
You're in your second month of pregnancy already – how exciting!
If you're following a pregnancy app or receive weekly updates, you know that your baby's brain, spinal cord, circulatory system, and so much more are beginning to form.
It's easy to read all of that and think your baby is incredible.
But let's pause for a minute and acknowledge that your body is doing this, your body is making this all possible.
YOUR BODY IS AMAZING!
Hold onto that truth as you prepare for your first prenatal visit which will usually happen between 6 – 8 weeks of pregnancy.
There might be conversations that take place during this appointment that make you question your body's ability to have a healthy outcome.
It's critical to connect with a size-friendly healthcare provider! That's someone who shares evidence-based information and recommendations in a manner that doesn't make you feel shame.
When it comes to intersectionality in care and outcomes, we know that being a person of size can be one of many marginalizations. For example, a Black plus size pregnant woman also faces racial biases in healthcare and the highest maternal mortality rate. When Black patients connect with Black doctors, it reduces their risks.
For those in BIPOC, LGBTQ+, and Disability communities, there's a lot more that comes into play with connecting with a care provider who is not only size-friendly but can support your individualized needs. Organizations like Black Birthing Bill of Rights, Elephant Circle, and DisAbilityMaternityCare provide support.
If there's anything we can do to help connect you to the resources you're searching for, please reach out!
When planning for prenatal visits, they commonly occur according to the schedule below. However, you might attend more based on a high-risk classification, if you have unique medical needs, or if your provider recommends additional screening. Whether or not those things happen are completely care-provider specific and/or necessary if any concerns come up during your pregnancy.
4 to 28 Weeks = 1 visit a month
28 to 36 Weeks = 1 visit every two weeks*
36 to 40 Weeks = 1 visit every week
* 2-week visits might start later in the third trimester if you're working with midwives.
Be sure to inquire with your care provider what they foresee for your prenatal care needs.
For example, it is common for people with a BMI over 30 to receive additional ultrasounds near the end of pregnancy if there are any concerns about the baby's size or function of the placenta. If you want to know what to expect, just ask!
Here's our guide to preparing for your first prenatal visit when you're plus size.
Week 6: Increased Risks


As you prepare for your first prenatal visit, you might dig into information online about all the increased risks during pregnancy with a larger body.
You'll read you have increased risks for conditions like gestational diabetes, gestational hypertension, preeclampsia, thrombosis, urinary tract infections, and sleep apnea.
For your baby, you’ll see concerns around having a baby that's large for gestational age, prematurity, congenital abnormalities, miscarriage, and stillbirth.
First, we've said this once, but we'll keep repeating it – just because there's an increased risk of developing a complication doesn't mean that you automatically will. Statistically speaking, you’re much more likely to have a healthy pregnancy than you are to experience these complications!
But also, the truth is, ALL people of ALL sizes can experience any of these complications in pregnancy – so please don't feel like you have done something wrong if it happens to you!
If you're focusing on your overall wellness and connecting with a care provider who helps you to feel supported – you're doing all you can to set yourself up for a healthy pregnancy outcome.
Let's revisit gestational diabetes (GD) for a minute as we discuss increased risks during pregnancy in a larger body.
Your care provider might recommend early screening for glucose tolerance during your first or second prenatal visit. Many people take the test, pass it, and then are confused around 24 – 28 weeks of pregnancy when they are informed they need to test again.
This first test is just to see if you're already pre-diabetic or diabetic. And if you've recently had your A1C levels checked, you can provide your care provider with your lab results (but they may still request you do the glucose screening).
Along with being tested twice, your care provider will likely talk to you about your increased risk of incurring GD. For example, they might tell you that you're four to five times more likely to develop GD than someone with a BMI of 25.
That's your relative risk. Relative risk is a rate compared to another rate.
But what does that mean? Yes, it tells you you're at a greater risk of developing GD, but by how much? Because “four to five times more likely” sounds kind of scary…
Your absolute risk percentage of incurring GD with a BMI over 40 is 17%.
We encourage you to look at that 17% as an 83% chance of not incurring GD.
And best of all, that number isn't even fixed because focusing on nutrition and physical activity throughout your pregnancy can reduce your risks even further.
In the My Plus Size Pregnancy Guide we go in-depth with plus size pregnancy risks and how to reduce your risks step-by-step.
Don't feel discouraged if your care provider reviews all of your increased risks. Instead, looking at the evidence can empower us to focus on healthy habits throughout pregnancy and beyond. And most often tests like the glucose screen in pregnancy end up being a confirmation of your health.
With that said, if your care provider is harping on risks, that may be a red flag that they aren’t actually size-friendly.
We encourage you to bookmark our go-to resource for evidence-based information during pregnancy and birth – Evidence Based Birth. You can also listen to our interview on the Evidence Based Birth Podcast, as well as when Rebecca Dekker, PhD, RN, was a guest on the Plus Mommy Podcast.
Week 7: Pregnancy Weight Gain Limits
As we covered in the guide for your first prenatal visit, the weight gain recommendation when you have a BMI over 30 is 11 – 20 pounds if you're carrying one baby and 25 – 42 pounds for twins or multiples.
It is not uncommon to experience a limited amount of weight gain during pregnancy when paying close attention to nutrition and physical activity when you have a BMI over 30.
Please note we didn't say anything about restricting or dieting. The key is focusing on nutrition and physical activity in a way that doesn't feel overwhelming.
The books below are also exceptional resources to support you with nutrition during pregnancy.
We also highly recommend connecting with a Health At Every Size® informed nutritionist whenever possible.
Some care providers never bring up the topic of weight, while others can't seem to stop mentioning it.
We believe that there's nothing wrong with having conversations about weight gain – it's all about how these conversations take place. These talks should happen in a manner that doesn't leave you feeling bad about yourself or lead to restrictive eating behaviors.
If your care provider wants you to lose weight or harps on your weight at each appointment, strongly consider getting a second opinion, or at least discussing a preference to focus on behaviors, not the scale. It's never too late to look into connecting with a size-friendly care provider.
If you're unable to switch care providers, here are helpful tips for going to the doctor when you're fearful of fat-shaming.
And don't forget that you have options for stepping on the scale!
Finally, many people find that bringing a support person with them can help tremendously if they feel overwhelmed during visits where weight is discussed in shaming ways. Sometimes there is comfort in numbers!
Week 8: Noninvasive Prenatal Screen
This might've come up at your first prenatal visit, but if it didn't, let's chat about noninvasive prenatal testing (NIPT). You'll likely be offered this around the 9th week of pregnancy.
NIPT is a blood test that analyzes DNA fragments floating in your bloodstream from your pregnancy. This screening can determine your baby's chance of having a chromosome abnormality associated with certain genetic conditions. It also identifies the sex chromosomes for male (XY) and female (XX).
For people with a high BMI, because you have a higher overall volume of blood, there can be a decreased amount of DNA fragments in your blood, and your results might show up as “no result.”
Don't worry if this happens!
You'll want to test again once you're further along, or your care provider might recommend additional testing like an amniocentesis.
Some providers recommend testing a little later in your pregnancy to increase the odds of getting accurate results. You can also request a Myriad Prequel Prenatal Screen, designed for people with a high BMI.
Week 9: Mental Wellness
Welcome to your plus size pregnancy at 9 weeks! Let's chat about mental wellness.
When we think about mental health throughout perinatal care, the focus is often on postpartum depression. However, with all the significant hormonal and life changes in pregnancy, it is also crucial to take care of your mental health now!
Talk with your provider, your therapist, your partner, or other supportive people in your life if you feel like your mental health is shifting. Let your care provider know right away if you have any physical or mental health concerns. No concern is too small!
Pregnancy is also an excellent time for you, your partner, or any adults in your home to learn about the signs to look for with postpartum depression and other postpartum mood disorders and how to act if you need support.
There is some data to show plus size people have higher rates of postpartum depression. And this may be due to the biases encountered in pregnancy and prenatal care. Another reason to have a size-friendly provider!
Remember, people of all sizes experience depression and anxiety during pregnancy – it just doesn't get talked about often enough.
We encourage you to bookmark our go-to resource for pregnancy and postpartum mental wellness: Postpartum.net.
Week 10: Doulas

You might be wondering why we're talking about hiring a doula during this first trimester plus size pregnancy resource.
Hear us out; now's a great time to look into hiring a doula! The earlier you connect with a doula during your pregnancy, the longer you get to enjoy all the benefits of doula support.
A labor doula provides physical, educational, and emotional support during pregnancy, birth, and the postpartum period. There are also postpartum doulas who exclusively support families during the period after their babes are born.
There are also antepartum doulas who support families experiencing a high-risk pregnancy or when someone is on bedrest, along with abortion and death doulas (and many doulas do a combination of all sorts of doula work).
A doula is not a medical professional. Instead, it's someone who receives in-depth training and has experience in birth, postpartum, and even loss.
While your partner or a loved one certainly can be there to support you throughout labor, we highly recommend considering at least interviewing a few doulas.
And don't just take our word for it, the ACOG states, “Published data indicate that one of the most effective tools to improve labor and delivery outcomes is the continuous presence of support personnel, such as a doula.”
Learn more about doula support and tips for affording a doula here – Do I Need a Doula?
Finding a doula who has experience working with plus sized clients is super important! First, a doula can help you navigate what to expect in your care prenatally. Then, during your birth, a doula helps advocate for you during labor and physically supports you with massage and position changes.
We have an ever-growing directory of size-friendly doulas and other professionals who support families over on sizefriendly.com.
Week 11: Aspirin for Preeclampsia Prevention




You'll find many great tips online for reducing the risk of preeclampsia, from drinking plenty of water to exercising regularly. But have you heard about taking aspirin daily if you're at an increased risk?
There was a double-blind study assigning 150 mg of aspirin daily or placebo to people starting between 11 and 14 weeks of pregnancy and continuing until 36 weeks of pregnancy.
The results?
In the aspirin group, the risk of developing preeclampsia before 37 weeks of pregnancy was reduced by 62%.
If your care provider hasn't already made this recommendation, this is a great conversation to bring up with them. As always, be sure to speak with your provider first before taking any medications (even aspirin) or supplements.
On a final note this week, since you're probably peeing all the time due to pregnancy, and drinking lots of water, here's one of our favorite pregnancy tips – lean forward to pee! It will help empty your bladder and maybe save you a trip to the bathroom.
Contact your care provider right away if you have any pain with urination or are concerned about having a urinary tract infection.
Week 12: Ultrasounds




During your plus size pregnancy at 12 weeks, you'll likely have your next prenatal visit so come prepared with all of your questions. You may or may not receive an ultrasound during this appointment.
Let’s address a few things to help you prepare for getting an ultrasound during your plus size pregnancy.
You likely had a transvaginal (internal) ultrasound during your first prenatal visit (or maybe you have had more than one). At least one transabdominal ultrasound (external) usually happens between 18 and 22 weeks (but sometimes sooner).
What's different about having an external ultrasound when you're plus size? Let's talk about it!
An external ultrasound uses sound waves directed at the abdomen to get a picture of the baby. Unfortunately, ultrasound waves have a more challenging time going through adipose (fat) tissue.
There's nothing wrong with your body.
The ultrasound machines at most care providers’ offices weren’t developed with your body in mind – and that's unfortunate.
The good news is that as your baby gets bigger, it's easier to see and for the ultrasound tech to get the measurements they need.
Your care provider will see if the external ultrasound gets the imagining they need. They might want to do a transvaginal ultrasound or refer you to a facility with more advanced technology for your ultrasound.
If they refer you to a specialist to get a level two ultrasound, be sure to inquire about the cost involved. If that's an obstacle, talk to your doctor about the option of waiting to have an ultrasound a week or so later when your baby is larger and your regular provider could get a better picture.
When preparing for an external ultrasound when you’re plus size, you'll want to make sure your bladder is very full. There’s science behind it, trust us.
You'll probably need to move your body into different positions. For example, if you have an apron belly, the tech or your care provider might ask you to lift your belly.
If it feels better for you, offer to lift your belly before they even ask to help avoid a potentially awkward conversation.
Beyond getting into different positions during external ultrasounds, it is also good to be prepared that the tech might press extremely hard on your body.
Please speak up! We often hear people who have been left bruised and stories of people who have been fat-shamed by ultrasound technicians. This is unacceptable!
You might experience some discomfort, but you shouldn't be in pain.
No medical personnel should shame you. If that happens, talk to your care provider or the clinical director of your selected facility. Consider logging a written complaint that can be added to the employee's file. Ask your provider to ensure you can be treated by someone else from now on.
Again, we hope you only have positive experiences, but we feel it's critical to prepare you for what might occur and remind you that you must advocate for yourself.
Think of it this way, if your child was in a lot of pain during a procedure or was being belittled by someone, you would absolutely speak up – so do the same for yourself.
You're so worthy!!!
This helpful resource reviews how many ultrasounds people typically get during pregnancy. Please note that, due to your BMI, your care provider might order additional ultrasounds to help determine your baby's size and positioning during the third trimester.
We hope you feel nothing but support and excitement during your ultrasounds. Below is an informative interview with an ultrasound technician to help you feel even more prepared!
Week 13: Plus Size Maternity Clothes & Necessities



It's the end of your first trimester, so you might be thinking about what maternity clothes you'll need as your pregnancy progresses. Or possibly wondering how to even find plus size maternity clothes!
Common advice is to keep wearing your everyday clothes or size up. But there's a lot to be said for that well-marketed belly band on maternity bottom!
You likely won't need maternity-specific items for weeks or even months to come. But, when you're ready, we've curated the most comprehensive guide to plus size maternity clothes!
We also have a list of 29 size-inclusive items for pregnancy, birth, and postpartum.
From a high-weight exercise/birth ball to a must-have peri bottle, you'll see a few of our favorites below.
And would you believe it, we've reached the end of your first trimester. So now it's time for your second trimester, where we'll focus on maternity clothes, feeling flutters, when to expect your bump to pop – and so much more!
First Trimester Plus Size Pregnancy References
- Hales, C. M., Carroll, M. D., Fryar, C. D., & Ogden, C. L. (2017). Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief, 288. Humphreys S. (2010). The unethical use of BMI in contemporary general practice. The British journal of general practice : the journal of the Royal College of General Practitioners, 60(578), 696–697. https://doi.org/10.3399/bjgp10X515548
- Tayebi N, Yazdanpanahi Z, Yektatalab S, Pourahmad S, Akbarzadeh M. (2018) The relationship between body mass index (BMI) and menstrual disorders at different ages of menarche and sex hormones. J Natl Med Assoc. 2018;110:440–7 https://www.sciencedirect.com/science/article/abs/pii/S0027968417301025?via%3Dihub
- Paula C Brady, Leslie V Farland, Elizabeth S Ginsburg, (2018) Serum Human Chorionic Gonadotropin Among Women With and Without Obesity After Single Embryo Transfers, The Journal of Clinical Endocrinology & Metabolism, Volume 103, Issue 11, November 2018, Pages 4209–4215, https://doi.org/10.1210/jc.2018-01057
- ACOG Committee opinion no. 549: Obesity in pregnancy https://pubmed.ncbi.nlm.nih.gov/23262963/
- S. Joy, N. Istwan, D. Rhea, C. Desch, and G. Stanziano, (2009) The Impact of Maternal Obesity on the Incidence of Adverse Pregnancy Outcomes in High-Risk Term Pregnancies, American Journal of Perinatology, vol. 26, no. 5, pp. 345–349, 2009. https://pubmed.ncbi.nlm.nih.gov/19067282/
- Carlson, N. S., Leslie, S. L., & Dunn, A. (2018). Antepartum Care of Women Who Are Obese During Pregnancy: Systematic Review of the Current Evidence. J Midwifery Women's Health, 63(3), 259-272. doi:10.1111/jmwh.12758 (https://pubmed.ncbi.nlm.nih.gov/29758115/)
- Bacon, L., Aphramor, L (2011) Weight Science: evaluating the evidence for a paradigm shift Nutr J. doi: 10.1186/1475-2891-10-9 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3041737/)
- Health At Every Size®
- Jones, C., & Jomeen, J. (2017). Women with a BMI >/= 30kg/m(2) and their experience of maternity care: A meta ethnographic synthesis. Midwifery, 53, 87-95. doi:10.1016/j.midw.2017.07.011 (https://pubmed.ncbi.nlm.nih.gov/28779644/)
- Zestcott, C. A., Blair, I. V., & Stone, J. (2016). Examining the presence, consequences, and reduction of implicit bias in health care: A narrative review. Group processes & intergroup relations : GPIR, 19(4), 528-542. doi:10.1177/1368430216642029 https://pubmed.ncbi.nlm.nih.gov/27547105/
- Shawe, J, Ceulemans, D, Akhter, Z, et al. (2019) Pregnancy after bariatric surgery: Consensus recommendations for periconception, antenatal and postnatal care. Obesity Reviews. 2019; 20: 1507– 1522. https://doi.org/10.1111/obr.12927
- Garcia-Valdes L, Campoy C, Hayes H, Florido J, Rusanova I, Miranda MT, McArdle HJ. (2015) The Impact of Maternal Obesity on Iron Status, Placental Transferrin Receptor Expression and Hepcidin Expression in Human Pregnancy. Int J Obes (Lond). 2015 Apr;39(4):571-8
- Farah N, Kennedy C, Turner C, O'Dwyer V, Kennelly MM, Turner MJ. (2013) Maternal Obesity and Pre-Pregnancy Folic Acid Supplementation. Obese Facts. 2013;6(2):211-5.
- Nithya Sukumar, Sean Wilson, Hema Venkataraman, & Ponnusamy Saravanan. (2015) Low Vitamin BV12 in Pregnancy is Associated with Maternal Obesity and Gestational Diabetes. Endocrine Abstracts 38 P206| DOI:10.1530/endoabs.38.P206
- Josefson JL, Feinglass J, Rademaker AW, Metzger BE, Zeiss DM, Price HE, Langman CB. (2013) Maternal obesity and vitamin D sufficiency are associated with cord blood vitamin D insufficiency. J Clin Endocrinol Metab. 2013 Jan;98(1):114-9. doi:
- Dencker, A., Premberg, Å., Olander, E. K., McCourt, C., Haby, K., Dencker, S., Berg, M. (2016). Adopting a healthy lifestyle when pregnant and obese – an interview study three years after childbirth. BMC Pregnancy and Childbirth, 16, 201. doi:10.1186/s12884-016-0969-x https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-016-0969-x
- Davenport MH, Ruchat SM, Poitras VJ, et al. (2018) Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1367‐1375. https://pubmed.ncbi.nlm.nih.gov/30337463/
- Physical Activity and Exercise During Pregnancy and the Postpartum Period, AGOC Committee Opinion Number 650, December 2015 https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2020/04/physical-activity-and-exercise-during-pregnancy-and-the-postpartum-period
- Cooper DB, Yang L. Pregnancy And Exercise. (2021) In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2021. PMID: 28613571. https://europepmc.org/article/NBK/nbk430821
- Deirdre K. Tobias SM, Cuilin Zhang, MD, PHD, Rob M van Dam, MD, PHD, Katherine Bowers, PHD, and Frank B. Hu, MD, PHD. (2011) Physical Activity Before and During Pregnancy and Risk of Gestational Diabetes Mellitus. Diabetes Care 2011 Jan; 34(1): 223-229 https://doi.org/10.2337/dc10-1368
- ACOG Committee opinion no. 548: Weight Gain During Pregnancy https://www.acog.org/-/media/project/acog/acogorg/clinical/files/committee-opinion/articles/2013/01/weight-gain-during-pregnancy.pdf
- Champion, M. L., & Harper, L. M. (2020). Gestational Weight Gain: Update on Outcomes and Interventions. Current diabetes reports, 20(3), 11. https://doi.org/10.1007/s11892-020-1296-1
- Rasmussen, K. M., Yaktine, A. L., & Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines (Eds.). (2009). Weight Gain During Pregnancy: Reexamining the Guidelines. National Academies Press (US) https://pubmed.ncbi.nlm.nih.gov/20669500/
- Muktabhant B, Lawrie TA, Lumbiganon P, Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 6. Art. No.: CD007145. https://pubmed.ncbi.nlm.nih.gov/26068707/
- Molyneaux, E., Poston, L., Ashurst-Williams, S., & Howard, L. M. (2014). Obesity and mental disorders during pregnancy and postpartum: A systematic review and meta-analysis. Obstetrics and gynecology, 123(4), 857-867. doi:10.1097/AOG.0000000000000170 https://pubmed.ncbi.nlm.nih.gov/24785615/
- LaCoursiere, DY., Barrett-Connor, E., O'Hara, MW., Hutton, A., Varner, MW (2010) The association between prepregnancy obesity and screening positive for postpartum depression doi: 10.1111/j.1471-0528.2010.02569 https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1111/j.1471-0528.2010.02569.x
- Pregnancy For Every Body https://www.nichd.nih.gov/ncmhep/initiatives/pregnancy-for-every-body/moms-to-be
- Coroyannakis, C., & Khalil, A. (2019). Management of Hypertension in the Obese Pregnant Patient. Current hypertension reports, 21(3), 24. https://link.springer.com/article/10.1007/s11906-019-0927-x
- Anderson, N. H., McCowan, L. M., Fyfe, E. M., Chan, E. H., Taylor, R. S., Stewart, A. W., Dekker, G. A., North, R. A., & SCOPE Consortium (2012). The impact of maternal body mass index on the phenotype of pre-eclampsia: a prospective cohort study. BJOG : an international journal of obstetrics and gynaecology, 119(5), 589–595. https://doi.org/10.1111/j.1471-0528.2012.03278.x
- Paladini, D. (2009), Sonography in obese and overweight pregnant women: clinical, medicolegal and technical issues. Ultrasound Obstet Gynecol, 33: 720-729. https://doi.org/10.1002/uog.6393
- Gestational Diabetes Diagnosis: What Now? A Helpful To-Do List! - October 18, 2023
- Navigating Miscarriage and Self-Blame as a Plus-Size Individual - October 16, 2023
- How much does your BMI increase the odds of shoulder dystocia? - August 11, 2023